Connect With Us
Blog
Items filtered by date: December 2022
Essential Stretches for Runners

Running is an invigorating way to stay fit, but it can put a lot of strain on your muscles and joints. Incorporating proper stretching into your routine is essential to enhance flexibility, reduce the risk of injuries, and improve overall performance. Start with a dynamic warm-up, such as leg swings or high knees, to prepare your muscles for action. Post-run, static stretches can help relieve tension. The classic calf stretch, hamstring stretch, and quadriceps stretch are vital for targeting major running muscle groups. To address hip flexibility, try the pigeon pose or a seated hamstring stretch. It is helpful to remember to focus on your core with exercises like the seated torso twist or the standing hip flexor stretch. Consistency is key, and regularly incorporating these stretches into your running routine can enhance your flexibility. It may also reduce the risk of injuries and contribute to a more comfortable and enjoyable running experience. If you would like additional information about effective running stretches, it is suggested that you consult a podiatrist who can provide you with the information you are seeking.
All runners should take extra precaution when trying to avoid injury. If you have any concerns about your feet, contact Afsha Naimat-Shahzad, DPM of Leander Foot & Ankle. Our doctor will treat your foot and ankle needs.
How to Prevent Running Injuries
There are a lot of mistakes a runner can make prior to a workout that can induce injury. A lot of athletes tend to overstretch before running, instead of saving those workouts for a post-run routine. Deep lunges and hand-to-toe hamstring pulls should be performed after a workout instead of during a warmup. Another common mistake is jumping into an intense routine before your body is physically prepared for it. You should try to ease your way into long-distance running instead of forcing yourself to rush into it.
More Tips for Preventing Injury
- Incorporate Strength Training into Workouts - This will help improve the body’s overall athleticism
- Improve and Maintain Your Flexibility – Stretching everyday will help improve overall performance
- “Warm Up” Before Running and “Cool Down” Afterward – A warm up of 5-10 minutes helps get rid of lactic acid in the muscles and prevents delayed muscle soreness
- Cross-Training is Crucial
- Wear Proper Running Shoes
- Have a Formal Gait Analysis – Poor biomechanics can easily cause injury
If you have any questions, please feel free to contact our office located in Leander, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Treat Your Toenail Fungus
While not a serious issue, toenail fungus, or onychomycosis, can be an embarrassing and uncomfortable condition to experience. Toenail fungus is often caused from public areas that harbor fungi and improper cleaning/drying of the foot. Once infected, the fungus grows deeper into the nail and can be very hard to get rid of.
There are different types of fungus that cause toenail fungus. Dermatophytes, yeasts, and molds are the most frequent forms of fungus to infect the toenail. Dermatophytes are the most common among the three. Symptoms associated with fungal nails include the discoloration of the toenail, brittleness, and in some circumstances, a smell. Pain is rarely a symptom caused by toenail fungus.
Diagnosis of fungal nails is generally a rather quick process. However podiatrists will make sure that the cause is not another condition such as lichen planus, psoriasis, onychogryphosis, or nail damage. Podiatrists will make use of fungal cultures and microscopy to verify that it is fungus.
While over-the-counter ointments are readily available, most are ineffective. This is due to the fact that the nail is very protective and that the fungus slips in between the nail plate and bed. Podiatrists can offer oral medication which currently provides the best results.
Ultimately, prevention is the best line of defense against toenail fungus. Avoid unsanitary public showers. If you do use a public shower, use shower shoes to provide your foot with protection. Once you are finished showering, make sure to thoroughly dry your feet. Fungi thrive in warm, dark, and moist places like sweaty, warm feet that are left dark in shoes all day.
Causes and Symptoms of Toenail Fungus

Toenail fungus, known as onychomycosis, is a common condition that results from exposure to an overgrowth of certain fungi in your toenails. These fungi, including dermatophytes and yeast, can be found naturally on the skin or in the environment, possibly as airborne spores. A contributing factor to toenail fungus is a warm and humid environment that promotes fungal growth. If your feet remain damp or sweaty for extended periods, these microbes can thrive and rapidly multiply, leading to an infection. Moreover, any crack or tear in the skin or nail can provide an entry point for the fungi, allowing them to penetrate deeper into the tissue. As the infection progresses, fungal debris accumulates under the nail, causing it to thicken and change color, typically turning yellow, brown, or white. Cracks may develop in the affected nail as it weakens. This infection can become progressively severe if left untreated. Recognizing the common symptoms early and seeking prompt treatment from a podiatrist is essential. If you believe you have toenail fungus, it is suggested that you seek the help of a podiatrist as quickly as possible.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Afsha Naimat-Shahzad, DPM of Leander Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our office located in Leander, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ingrown Toenail Care
An ingrown toenail is a nail that has curved downward and grows into the skin. This typically occurs at the nail borders, or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. Milder cases that don’t involve infection or other medical conditions can benefit from soaking the feet in room-temperature water and gently massaging the side of the nail. In most cases, however, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Do Not Ignore Ingrown Toenails

Even if it does not cause pain, it is recommended that one does not ignore an ingrown toenail. Ingrown toenails happen when the corner or side of the toenail grows into the surrounding flesh, leading to pain, discomfort, inflammation, and sometimes infection. Initially a minor annoyance, untreated ingrown toenails can escalate into a recurring and serious issue. Treatment methods depend on the ingrown toenail's severity, the presence of infection, and previous treatments that were attempted. Routine podiatry care, including toenail trimming and addressing underlying issues, can help prevent infected ingrown toenails. Options range from daily foot soaking and antibiotics to more invasive nail avulsion procedures, which involve removing the affected toenail. If you have an ingrown toenail, it is strongly suggested that you make an appointment with a podiatrist for treatment.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact Afsha Naimat-Shahzad, DPM of Leander Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our office located in Leander, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What to Know About a Broken Toe
The forefoot is composed of five metatarsal bones and fourteen phalanges. Each toe has three phalanges except for the big toe which only has two. Our toes play an essential role to the walking process, which is why a broken toe could seriously disrupt one’s ability to move around. Toe fractures are common and can be very painful. Fortunately, these injuries rarely require surgery and usually heal with rest and a change in activity.
Broken toes typically result from a traumatic event such as falling, stubbing the toe, or dropping something on the toe. Traumatic toe fractures may be categorized as either minor or severe fractures. At times, one may hear a “pop” or “crack” sound when the bone breaks. Common symptoms of a traumatic toe fracture include pain, throbbing, bruising, swelling, and redness.
Another type of toe fractures is a stress fracture. These injuries usually appear in the form of small hairline breaks on the bone. Stress fractures develop after repetitive activity instead of a single injury. Stress fractures occur when the muscles in the bone become too weak to absorb impact. Consequently, the toe bone becomes vulnerable to any pressure and impact it endures. Symptoms for a stress fracture in the toe include swelling without bruising, tenderness to the touch, pain that goes away with rest, and pain after walking or running.
If you suspect that you have a broken toe, you should make an appointment with your podiatrist. He or she will likely diagnose you by performing a physical exam and an X-ray. Treatment for a broken toe may include the R.I.C.E. method, buddy taping, surgery, or antibiotics. The R.I.C.E. method (Rest, Ice, Compression, and Elevation) is a common treatment method for many injuries because it decreases pain. Buddy tapping involves wrapping the injured toe next to an adjacent toe to keep it supported and protected. These two methods have proven to be effective in the healing process for toe fractures. The estimated healing time for a broken toe is approximately four to six weeks. If the injury becomes infected or requires surgery, the estimated healing time may take eight weeks or more.
Signs and Treatments for a Broken Toe

A broken toe, though relatively common, can be a painful and inconvenient injury. Knowing the signs and how to address them can expedite the healing process and prevent potential complications. Signs of a broken toe typically include immediate pain, swelling, bruising, and difficulty in moving the affected toe. In some cases, you may even hear or feel a snap or pop at the time of injury. If you suspect a broken toe, it is important to seek medical attention promptly. Having an X-ray and a physical examination performed is generally successful in diagnosing a broken toe. Treatment for a broken toe often involves immobilization, which may include splinting, or buddy taping, which is taping the injured toe to a neighboring toe. Additionally, it may be beneficial to wear a protective boot that can also provide stability and mobility. Pain management measures, such as taking over the counter pain relievers and elevating the foot, can help to alleviate discomfort and reduce swelling. Recovery time varies but typically ranges from a few weeks to a couple of months. Recognizing the signs and seeking timely treatment are essential steps toward healing a broken toe effectively and minimizing long-term issues. If you have broken your toe, it is suggested that you make an apppointment with a podiatrist who can guide you toward the correct treatment option.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact Afsha Naimat-Shahzad, DPM from Leander Foot & Ankle. Our doctor will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact our office located in Leander, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
Facts About Heel Spurs
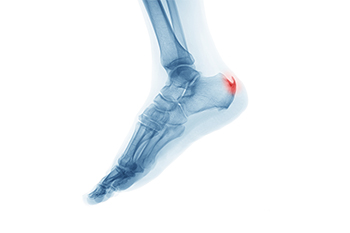
Heel spurs, though commonly misunderstood, are a prevalent foot condition that affects many individuals. These bony growths form on the underside of the heel bone and often coexist with another foot issue, such as plantar fasciitis. Contrary to popular belief, heel spurs themselves may not always be the primary source of pain. Instead, it is the inflammation and irritation of the surrounding tissues that typically cause discomfort. Heel spurs often develop due to excessive strain and stress on the heel, which can result from factors such as obesity, wearing improper footwear, or repetitive activities. While they can be detected through X-rays, treatment usually targets the underlying condition. Conservative approaches consisting of rest and wearing orthotic inserts, may help to alleviate symptoms. In rare cases, surgery may be considered when conservative methods prove ineffective. Understanding the facts about heel spurs can help individuals make informed decisions about their foot health and seek appropriate treatment when needed. If you have heel pain, and suspect it may be a heel spur, it is suggested that you visit a podiatrist who can accurately diagnose and treat the problem.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Afsha Naimat-Shahzad, DPM from Leander Foot & Ankle. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Leander, TX . We offer the latest in diagnostic and treatment technology to meet your needs.
Why Live with Pain and Numbness in Your Feet?
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022